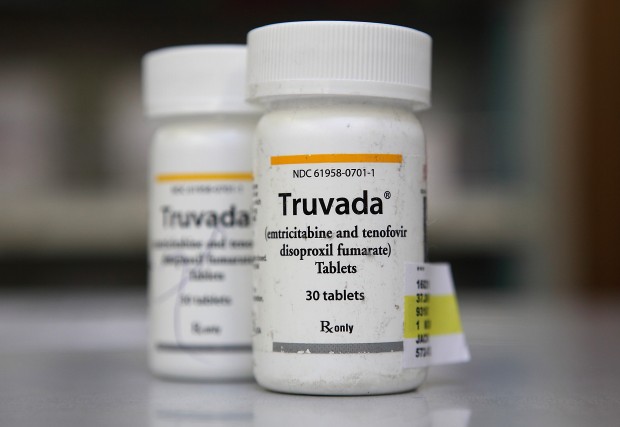
The Food and Drug Administration approved Truvada for PrEP in 2012. The drug is more than 90 percent effective at preventing HIV infection. But critics worry that use of Truvada may lead to reckless sexual behavior and continued spread of the virus.
But Grant's continuing research on Truvada has shown no new infections in people who take the pill daily. What’s more, Grant told the assembled audience that those who need PrEP most are seeking it out and taking it.
“There’s been some fear that PrEP would release a storm of sexuality, where people will have more partners,” he said. “What we’ve found is that the opposite is true. Those who take PrEP become more mindful of their sexual goals. They become more talkative with their partners about HIV risks and other (sexually transmitted illnesses).”
But while PrEP seems effective, only 2,319 people received prescriptions of Truvada for PrEP nationwide between 2012 and 2013, according to data from Gilead Sciences, which makes the drug. Grant said that a “tipping point” came in late 2013, where more people began to know about and request Truvada for PrEP, but that’s still a far cry from the 500,000 Americans that the Centers for Disease Control say could benefit from the prevention method.
Some of that disconnect may be due to cost. A year of Truvada runs about $13,000 without insurance. While Medi-Cal, Healthy San Francisco, and the majority of private insurers cover Truvada for PrEP, many people at highest risk for HIV —- young African American men who have sex with men, transgender women, sex workers, straight women and gay men in long-term relationships with HIV-positive partners, or gay men who are dating or in open relationships —- often have no insurance or have opted for insurance with high deductibles or scant drug coverage, putting a Truvada prescription out of reach for many.
Erik Gibb said he considers himself to be a “lucky guy” when it comes to PrEP, even though his health plan includes a $3,000 deductible and a $3,600-a-year copay for his Truvada prescription. Another speaker, Eric Norman, said he and his partner, an HIV-positive man, once had a scare, and Norman was worried he had contracted HIV. He was able to get a combination of stronger antiretroviral drugs which successfully prevented infection. He wanted to start on PrEP, but didn't have insurance and could not afford the medication.
“So I went back to this relationship, and I was happy in it,” he said. “But I was still living with the fear of infection and the risk that I was going to become HIV positive.”
Under Campos' proposal, about $500,000 would go toward drug copay assistance.The rest would pay for hiring and training community navigators, who can help those in need of Truvada navigate the insurance system and get the treatment fully covered.
Supervisor Scott Weiner, who announced Wednesday that he’s one of the 1,000 San Franciscans taking Truvada for PrEP, said that access to PrEP shouldn’t be limited just to those who have access to good insurance.
Before the hearing Thursday morning, Campos led an assembly on the steps of City Hall in a moment of silence for all those lost to the virus.
“We owe it to them,” he said, “to make sure no one else gets infected.”
Heather Boerner is a San Francisco-based healthcare journalist and author of Positively Negative: Love, Pregnancy, and Science’s Surprising Victory Over HIV.